2020 saw the launch of an emotional support service on the neonatal intensive care unit, funded by the charity’s Tiny Lives Appeal. Here, Noah’s Ark neonatal principal psychologist, Catriona Matthews, explains a little bit more about how the service supports parents and staff.
 “Having a child on NICU is an incredibly traumatic and distressing experience, whether that child is premature or full term, and whether they spend hours, days or months on the unit. It is not how parents imagined welcoming their baby into the world and, as well as dealing with seeing their baby so fragile and undergoing necessary but invasive procedures, they are having to come to terms with the loss of the pregnancy, birth and first family moments they had imagined. This is a huge amount to deal with while also trying to work out how to be a parent and care for their babies.
“Having a child on NICU is an incredibly traumatic and distressing experience, whether that child is premature or full term, and whether they spend hours, days or months on the unit. It is not how parents imagined welcoming their baby into the world and, as well as dealing with seeing their baby so fragile and undergoing necessary but invasive procedures, they are having to come to terms with the loss of the pregnancy, birth and first family moments they had imagined. This is a huge amount to deal with while also trying to work out how to be a parent and care for their babies.
While the NICU staff do a fantastic job of trying to support families emotionally, they have to balance this with providing the medical care and support that babies need. In my role I have the specialist training and dedicated time to commit to these families to help them to explore their experience and feelings and think about how best to cope during an unbelievably difficult time. Being able to make sense of their experience in some helps parents feel in a better place to be able to provide the care and loving relationship which is so important to their babies.
 Becoming a parent is a huge challenge for everyone but NICU parents are doing this whilst dealing with many additional stresses and difficulties. They may feel frightened to touch or hold their baby, worry there is nothing they can do to care for them or feel worried that they don’t feel an “instant bond” with their baby. COVID has added to these difficulties by preventing mothers from being able to have their partners or family alongside them supporting them through this challenging time. Within my role, I can help parents talk about and normalise the range of feeling and worries they have about their baby and becoming a parent.
Becoming a parent is a huge challenge for everyone but NICU parents are doing this whilst dealing with many additional stresses and difficulties. They may feel frightened to touch or hold their baby, worry there is nothing they can do to care for them or feel worried that they don’t feel an “instant bond” with their baby. COVID has added to these difficulties by preventing mothers from being able to have their partners or family alongside them supporting them through this challenging time. Within my role, I can help parents talk about and normalise the range of feeling and worries they have about their baby and becoming a parent.
My role is to provide a space which is completely focused on hearing and understanding their story so they don’t need to worry about distracting me from the medical tasks as they might with a doctor or nurse. A psychologist’s training and experience also means we have specialist skills to help us to be alongside and understand parent’s distress and offer ideas and strategies to help them to cope with all that they are dealing with during their NICU journey.
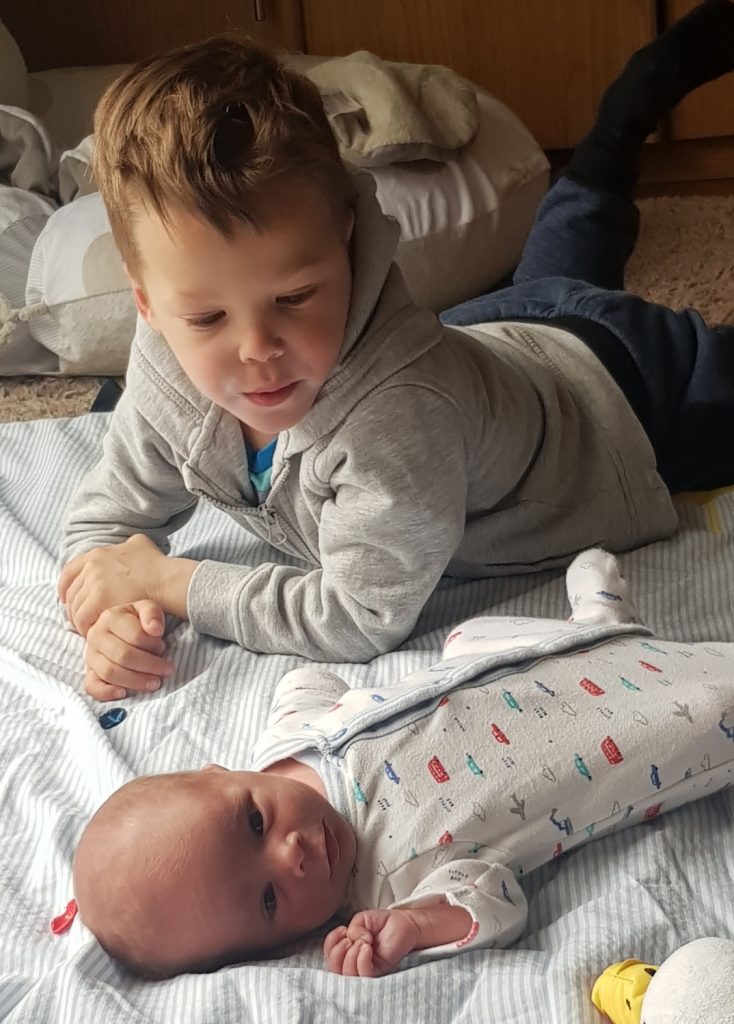
But we know too that the neonatal journey doesn’t end when parents go home. Their experience can continue to impact them for months or even years after leaving hospital. I invite parents to contact me if they need support and we’re currently looking to establish a group to support parents with some of the common difficulties they may face when returning home with their babies.
Very sadly, not all babies do get the chance to go home and on the traumatic occasions where a baby on the unit dies, I am also able to offer bereavement support. This may involve allowing parents to talk through the story of their baby’s life and death, providing support to siblings, finding ways of marking important dates or developing ways of coping with the range of overwhelming emotions in response to losing a baby. All parents face the challenge of finding a way to balance loving and grieving their baby alongside continuing to live their life.
In order to give the medical and emotional care which families need, it’s important that staff themselves also feel supported. Although working in NICU can be hugely rewarding, seeing babies and families in distress can also be challenging for staff. So another part of my role is to support the emotional wellbeing of the NICU team through offering group and one to one support. This in turn means that they are able to provide the best possible support to babies and families.”
 Tarnia Lewis had her first experience of the neonatal intensive care unit when her son Aiden was born 11 weeks early four years ago. Though she can’t praise the care Aiden received highly enough, she describes the experience as very difficult and traumatic and one that both she and her husband, Craig struggled with for quite some time after.
Tarnia Lewis had her first experience of the neonatal intensive care unit when her son Aiden was born 11 weeks early four years ago. Though she can’t praise the care Aiden received highly enough, she describes the experience as very difficult and traumatic and one that both she and her husband, Craig struggled with for quite some time after.
Recently, Tarnia got to experience the new neonatal intensive care unit when her third child Addison was born at 34 weeks of pregnancy. This time, Tarnia was offered support by Catriona and it was an opportunity she felt very grateful for.
Tarnia says: “When I was in NICU with Aiden, the only opportunity we had to try and process what had happened was a de-brief before discharge but that was very medically focussed. As a NICU parent you struggle to understand your experience and both how and why it happened. You blame yourself and though you try to talk to family and friends, it’s difficult for them to relate and they don’t understand the full impact of having a baby on NICU. Having someone like Catriona within that environment who understands and is there expressly to support you emotional is so important.”
 Olivia Spicer, who is mum to baby Teddy, also benefited from the support of the emotional support service after a particularly traumatic birth in December 2020. Teddy was rushed to the neonatal intensive care unit with a collapsed lung and, still very unwell herself, Olivia spent six days at her son’s cotside before he was discharged. Olivia spent an additional week in hospital without her baby.
Olivia Spicer, who is mum to baby Teddy, also benefited from the support of the emotional support service after a particularly traumatic birth in December 2020. Teddy was rushed to the neonatal intensive care unit with a collapsed lung and, still very unwell herself, Olivia spent six days at her son’s cotside before he was discharged. Olivia spent an additional week in hospital without her baby.
Olivia says: “Nothing can prepare you for the experience of having your newborn baby on intensive care but I’ll never forget how kind and helpful Catriona was. She even followed up with calls after we were discharged which has given me the opportunity to work through some of the really traumatic memories I have. I think I would be in such a different place mentally now if I hadn’t had that support and I find it hard to even imagine how much harder the experience would have been without it.”







